Patient Bill of Rights and Patient Rights in Healthcare Research
If you’re considering participating in a clinical trial, you might be curious about what rights you have as a patient, and what patient protections are in place to keep you safe. In this article, we’ll provide a quick summary of patient rights in healthcare research and the different safeguards that exist to prioritize your safety and make sure your basic rights are respected.
Patient rights in healthcare research
Clinical research studies and clinical trials are scientific studies that represent a key method for learning more about health conditions and assessing the safety and effectiveness of new medical interventions like drugs and therapies.
Since clinical research involves living human beings as research subjects, there is a major underlying focus on maintaining strong ethical research practices and protecting patient safety and wellbeing.
Patient safety and research ethics principles are set forth in varying guidelines and regulations and enforced through different means:
- Informed consent and consenting procedures
- Third-party review of research protocols and study materials by independent review boards (IRBs)
- Guidelines and regulations set forth in the Code of Federal Regulations (CFR), overseen and enforced by government agencies:
- Title 21 CFR, set forth by the Food and Drug Administration (FDA)
- Title 45 CFR part A (“the Common Rule”), set forth by the Department of Health and Human Services (HHS)
- The Health Insurance Portability and Accountability Act (HIPAA)
- Good Clinical Practice (GCP) guidelines set forth by the ICH
Further reading
→ For a deeper look at clinical trial regulations and guidelines, including CFR Titles 21 and 45, GCP, and IRB approvals, have a look at our explainer on clinical trial regulatory compliance:
Regulatory Compliance in Clinical Research | Power
→ To read more about clinical research ethics on a broader level, see:
https://www.withpower.com/guides/clinical-research-ethics
→ For more on data confidentiality and privacy in clinical trials, see:
Data Privacy in Clinical Trials: Standards, Definitions, and Best Practices | Power
Patient rights in clinical trials
Patient rights and responsibilities in a clinical trial are laid out as part of the clinical trial protocol – the “master document” describing exactly what a study involves and how it will be conducted. The study protocol is reviewed by both an IRB and the FDA before it is authorized to proceed. Part of this review involves ensuring that the study strictly upholds patient rights and takes adequate steps to safeguard their safety and well-being.
Specific patient rights in clinical trials include:
1. Informed consent
Participants have the right to receive clear and detailed information about the purpose of the trial, its potential risks and benefits and what is required of them, alternative treatment options that may be available apart from the trial, and any compensation or reimbursement provided. Participants should have ample time to consider participation, including being able to ask questions and to discuss it with their family/friends/doctor/etc.
2. Right to withdraw
Participants in a clinical trial have the right to withdraw from the study at any time, without penalty and even without needing to provide an explanation.
3. Confidentiality
Participants have the right to privacy regarding their participation and any personal health information that is collected during a clinical trial. Researchers must comply with data protection laws such as HIPAA in handling participant data (more on this below).
4. Safety monitoring
Participants have the right to adequate safety monitoring throughout the duration of the study. The sponsor is responsible for making sure there is a solid monitoring program in place, involving an ongoing assessment of potential risks to patient safety and indications of possible adverse events, which must be addressed promptly. When a severe adverse event occurs, the study may be paused or stopped until it can be clarified whether the adverse event was related to the study intervention.
5. Access to medical care
Participants should continue to receive appropriate medical care for their condition, as they would normally, even while participating in a clinical trial. Thus, the study should not jeopardize the patients’ access to any treatments deemed necessary that fall outside of the research protocol setting.
6. Respect and dignity
Participants are entitled to be treated respectfully and with dignity, without discrimination or exploitation based on factors such as age, gender, race, ethnicity, socioeconomic status, disability, or their medical condition.
7. Transparent communication
Researchers are expected to maintain ongoing communication with participants regarding any significant findings or updates that may impact their decision to remain in a study. This could include the development of potential severe adverse events or complications in other participants.
8. Compensation for injuries
If participants experience harm as a result of their involvement in a trial due to negligence or unforeseen complications related directly to the trial or the intervention under study, they are entitled to compensation for those injuries directly resulting from their involvement in the trial.

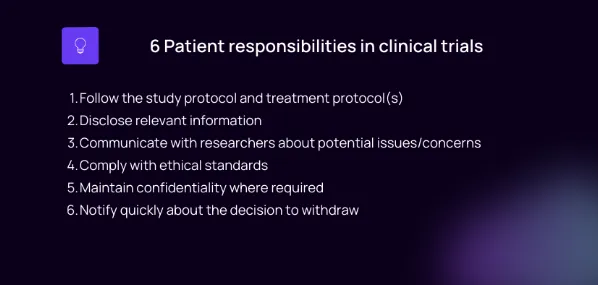
While patients have many rights as we’ve seen above, they also have certain responsibilities to be aware of when taking part in a clinical trial. While research sponsors and investigators must uphold their obligations to ensure participant safety and well-being, participants also hold responsibilities towards the study and its objectives. These will be outlined clearly in the trial protocol and in the informed consent form.
Specific patient responsibilities in clinical trials include:
1. Following the study protocol
Participants are expected to adhere to the instructions provided by the research team, including attending scheduled visits, taking any medications as prescribed, completing questionnaires or assessments accurately and on time, and reporting any changes in their health status. Other specific requirements may exist, and will be outlined clearly in the research protocol and explained during the informed consent procedure.
2. Disclosure of relevant information
It is crucial for participants to openly share all pertinent medical history and information with the research team, in order to enable an accurate and truthful assessment of their eligibility for the trial and to support appropriate monitoring during participation. Providing this information is vital for patient safety, as pharmacological interventions tend to have an extensive list of potentially dangerous interactions (contraindications) with certain health characteristics, genetics, habits, other medications, and even food and supplements.
3. Active communication
Participants should maintain open communication with the research team by voicing any concerns or questions they may have throughout the trial duration. This includes promptly reporting any changes in their health or unanticipated effects that may or may not be related to the study intervention.
4. Complying with ethical standards
Participants also play a role in upholding ethical research practices during a clinical trial by making sure not to misrepresent facts, falsify data, or engage in behaviors that might compromise the integrity of the study (see next point).
5. Confidentiality and privacy
Participants are responsible for maintaining confidentiality regarding any sensitive information that is shared with them by researchers, within group sessions, or through interactions with other participants. This can include information about treatment assignments, the nature of the study drug, etc. – any information that is considered confidential will be indicated as such to the participant during the informed consent procedure and as it arises during the trial.
6. Withdrawing consent if desired
If a participant wishes to withdraw from the study at any point during a clinical trial, they have the right to do so, as discussed above. However, they also have the responsibility to communicate this decision promptly with the research team, as high attrition (drop-out) rates can have a negative effect on the trial, and in some cases the research team may need to enroll a new patient promptly to maintain an adequate sample size to allow them to answer the research question accurately. Further, some interventions may require the patient be weaned off slowly, or they may require continued health monitoring for some time after stopping treatment – this is also thus a question of patient safety.
What is the patient bill of rights?
Oftentimes, complete patient rights are laid out formally in a document known as a patient bill of rights. Patients’ bill of rights can exist at federal, regional, or institutional levels.
One example is the American Hospital Association (AHA)’s Patient’s Bill of Rights which was set forth in 1973 (and later updated in 1992). The AHA’s Patients’ Bill of Rights outlined guidelines for hospitals to ensure they were treating patients fairly, and also to guide patients on participating actively in their healthcare and communicating complaints or concerns. The AHA updated this guidance in 2003 to a more concise list called The Patient Care Partnership. A copy of the Patient Care Partnership outlining patients’ rights during a hospital stay can be accessed through the following link:
https://www.aha.org/system/files/2018-01/aha-patient-care-partnership.pdf
The basic patient rights outlined in the AHA’s Patients’ Bill of Rights are:
- High quality hospital care
- A clean and safe environment
- Involvement in your care
- Protection of your privacy
- Help when leaving the hospital
- Help with your billing claims
Another well-known patient bill of rights is the National Institutes of Health (NIH) Clinical Center Patients’ Bill of Rights, which applies to all clinical research studies conducted by the NIH Clinical Center. The NIH Clinical Center Patient Bill of Rights can be accessed here:
https://clinicalcenter.nih.gov/sites/nihinternet/files/internet-files/participate/_pdf/bor.pdf
The Affordable Care Act (ACA) was enacted in 2010, and later a Patients’ Bill of Rights was developed which applies to healthcare coverage. More information on the Patients’ Bill of Rights can be found by following the links contained on this landing page:
https://www.cms.gov/marketplace/private-health-insurance/patient-bill-of-rights
Patient rights under HIPAA
The Health Insurance Portability and Accountability Act – or HIPAA – is a U.S. federal law enacted in 1996 designed to safeguard patients' protected health information (PHI). HIPAA primarily governs privacy practices in electronic healthcare transactions within healthcare facilities, and is not specifically targeted to clinical trials, but it increasingly applies to clinical trials as technological integration accelerates.
Under HIPAA regulations, patients have several key rights regarding their protected health information (PHI):
1. Right to access: Patients have the right to obtain copies of their medical records and request amendments or corrections to inaccurate or incomplete information.
2. Right to privacy: Patients have the right to expect that their medical information is kept private and accessed only for uses necessary for healthcare purposes, or as otherwise permitted under HIPAA regulations.
3. Right to control disclosure: Patients can control who has access to their health information through written authorization, such as when participating in a research study wherein PHI may be shared with researchers.
4. Right to notice of privacy practices: Patients have the right to receive a notice from covered entities (the healthcare bodies covered under HIPAA) explaining how their PHI is used, disclosed, and protected.
It is important for research institutions conducting clinical trials to understand and adhere to HIPAA regulations, particularly in the case of trials employing electronic systems and managing electronic health data (which is now the majority of modern trials).
Examples of patient rights violations
Some situations that would exemplify violations of patient rights in clinical trials include:
1. Inadequate informed consent: Failing to provide complete information about the nature of the study, its potential risks and benefits, and alternative treatment options represents a failure to obtain fully informed consent. While IRB approvals today pay particular attention to informed consent procedures and such a situation is less likely to occur, there have been instances in the past such as the famous Tuskegee trials, wherein patients with syphilis were studied without being informed about the nature of the study.
2. Breach of confidentiality: Inappropriate handling or accidental disclosure of participant information can compromise patient privacy and represents a violation of their confidentiality and privacy rights. An example could include revealing a participants’ participation in a study to their employer, or revealing their full name to an unauthorized third party.
3. Coercion or undue influence: Pressuring, manipulating, or coercing individuals into participating in a clinical trial undermines the voluntary nature of participation, and would be a clear violation of basic patient rights.
4. Discrimination: Treating participants differently based on characteristics such as age, gender, race, ethnicity, socioeconomic status, or disability violates principles of equity and fairness. Here, it is important to note that eligibility criteria are established to optimize the quality of the research design and protect certain populations from undue risk – filtering participants based on fairly designed inclusion and exclusion criteria does not constitute a violation of patient rights nor unethical conduct.
5. Negligence leading to harm: Failure to perform sufficient safety monitoring or to address unforeseen complications or adverse events in a timely manner can have potentially serious consequences for participants, and is considered unethical and a violation of the patient's right to ethical treatment.
6. Non-consensual continuation: If a participant decides to withdraw from a study voluntarily due to concerns about their health or other reasons but is not allowed to do so by researchers against their wishes; it represents a violation of their autonomy and right to discontinue participation at any time without penalty.
Conclusion
Participating in a clinical trial is a decision that deserves thorough consideration, and which ultimately is up to you, the patient. You will be given full and complete information about the purpose of the study and what is required of you, including potential risks and alternative options you have, before you are asked to decide whether to participate. We hope that this article has helped you understand the numerous protections that are in place to ensure you are treated fairly and ethically. Your participation is important to researchers, and it is their responsibility to take all possible reasonable action to ensure your safety.