Learn More About Crohn's Disease Research Studies
What Are Crohn's Disease Clinical Trials?
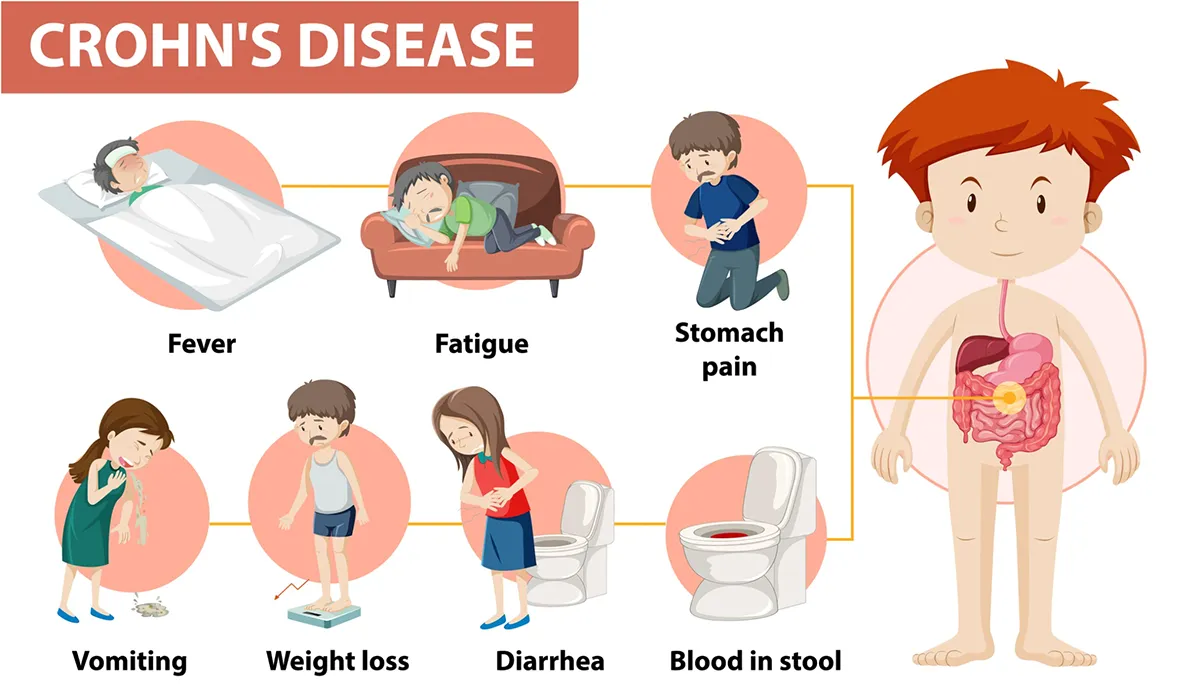
Crohn’s disease is a chronic inflammatory condition that affects the gastrointestinal tract with increasing prevalence in the world. It leads to the inflammation of the tissues in the digestive tract, which can cause severe diarrhea, abdominal pain, weight loss, and fatigue, among others. The swelling caused by Crohn’s disease affects different areas of the digestive tract in different people, especially the small intestine.
The inflammation may spread into deeper layers of the bowel. Crohn's disease can be very painful for patients and adversely affects their quality of life. There is no cure for Crohn's disease and health practitioners are primarily focused on managing its symptoms, minimizing the inflammation, and bringing about long term remission. Many patients with Crohn's disease can improve their quality of life.
Crohn’s disease research trials are aimed at learning about its pathophysiology, including its primary cause. Researchers have highlighted a number of factors for increasing the risk of Crohn’s disease, including microbial, environmental, genetic, vascular, and psychosocial factors. Smoking and the use of NSAIDs may also increase a person's likelihood of Crohn’s disease. Other areas of research include lifestyle habits and the impact of certain food groups on inflammation.
Why Is Crohn's Disease Being Studied Through Clinical Trials?
Researchers are improving their understanding of Crohn’s disease and what triggers the painful conditions. They are also studying new ways of diagnosing, tracking, and treating Crohn’s disease in an effective manner. Researchers have observed that industrialization and a western lifestyle are linked to Crohn’s disease.
It is imperative to develop novel treatment modalities that help manage Crohn’s disease without increasing the patient's risk of developing adverse side effects. Diagnostics is an important area of research in Crohn’s disease because its symptoms vary from person to person. It doesn’t help that Crohn’s disease shares similar symptoms with other intestinal disorders.
Weight loss, skin problems, and pain are also found in other symptoms. The current body of research is focused on finding more accurate tools to help health practitioners definitively diagnose Crohn’s disease.
Early diagnosis is crucial for managing symptoms and preventing the inflammation from spreading to other parts of the body. Failing to manage the symptoms of Crohn’s disease can lead to severe complications, including colon cancer, fistulas, bowel obstructions, and anal fissures.
What Are The Types of Treatments Available For Crohn's Disease?
Treatment for Crohn’s disease largely depends on the patient’s symptoms. Doctors will carry out a number of tests to determine the severity of the inflammation. Blood tests are often used to check for white blood cells because it indicates inflammation. The test also checks for anemia because many patients with Crohn’s disease have a low red blood cell count.
A stool test may be carried out to rule out infections that could be causing other diseases. Doctors also use biopsies to look for signs of inflammation. These tests may be combined with CT scans, endoscopy, and X ray images to provide a definitive diagnosis of Crohn’s disease.
Antibiotics are the first line of treatment for Crohn’s disease because they play an important role in preventing infections. This is followed by anti diarrhea medication to stop severe diarrhea commonly associated with Crohn’s disease. Patients may be asked to fast for several days or longer to help their intestines heal. Nutrition may be provided through intravenous methods.
Doctors manage inflammation in patients with the aid of corticosteroids and may combine it with immunomodulators to suppress the immune system. Drugs such as cyclosporine and azathioprine are commonly prescribed. If symptoms don’t improve or get worse with time, doctors may have to conduct surgery to correct any blockages or bleeding.
What Are Some Recent Breakthrough Clinical Trials For Crohn's Disease?
Crohn’s disease clinical trials will help researchers and doctors understand the pathophysiology of the painful condition and help them develop novel treatment modalities. Below are major breakthrough studies in Crohn’s disease that have improved diagnostics, therapy, and remission rates.
1999: Infliximab for Treating Fistulas in Patients with Crohn’s Disease - This clinical trial investigated the use of infliximab, a chimeric monoclonal antibody, for treating Crohn’s disease. 94 patients with perianal fistulas were enrolled in the study. The participants were randomized and assigned to one of three treatments; 5mg of infliximab per kg of body weight, placebo, or 10 mg of infliximab per kg of body weight. Mediation was to be delivered intravenously at intervals of weeks 0, 2, and 6. The endpoint of the study was a reduction of 50% of more draining fistulas. The secondary endpoint was the closure of all fistulas.
68% of the patients who received 5 mg of infliximab per kg body weight and 56% of those who received 10 mg of infliximab per kg of body weight achieved the primary end point, compared with only 26% of patients in the placebo group. Moreover, 55% percent of patients on a lower dosage of infliximab compared to 38% on a higher dosage of infliximab had closure of all fistulas. This is compared to 13 percent of patients assigned to placebo. Adverse events were reported in 60% of all patients, with headache, fatigue, and upper respiratory tract infection being very common.
2015: Crohn’s Disease Management After Intestinal Resection - This randomized trial investigated various strategies to prevent postoperative disease recurrence after intestinal resection. Patients from 17 centers in New Zealand and Australia were scheduled to undergo intestinal resection for Crohn’s disease. Patients at a high risk of recurrence were prescribed adalimumab or thiopurine. Participants were randomized into parallel groups: colonoscopy at 6 months and no colonoscopy.
Researchers used computer generated block randomization to allocate patients to active or standard care. It was found that endoscopic recurrence occurred in 49% patients in the active group and 67% patients in the standard care group. 22% of the patients in the active care group maintained complete mucosal normality compared to just 8% in the standard care group. The researchers concluded that treatment with early colonoscopy may yield better results than conventional drug therapy for preventing a postoperative recurrence.
2019: Impact of an Exclusion Diet on Crohn’s Disease - Adolescents with mild to moderate symptoms of Crohn’s disease are usually prescribed exclusive enteral nutrition (EEN), however it can be very challenging to follow. In this randomized clinical trial, patients compared the results of EEN with the CD exclusion diet (CDED) along with partial enteral nutrition (PEN). This diet eliminates various dietary food groups that could adversely impact the patient’s intestinal barrier and microbiome.
Children were randomized into a group that received CDED for 6 weeks followed by CDED with 25% PEN or a group that only received EEN for 6 weeks. Various laboratory tests were performed to help researchers measure an outcome, including 16s ribosomal RNA gene (V4V5) sequencing on stool. Other endpoints were remission and corticosteroid free remission.
30 of 40 children in the CDED and PEN group were in corticosteroid free remission compared to just 20 of 34 in the EEN group. Moreover, the CDED and PEN group was also associated with reductions in inflammation and fecal proteobacteria. Although both diets are useful in managing the symptoms of Crohn’s disease, CDED plus PEN induced significant better results.
2021: Comparing Carbohydrate Diet with the Mediterranean Diet - This randomized clinical trial compared the results of the Specific Carbohydrate Diet (SCD) with the Mediterranean Diet (MD) for treating Crohn’s disease in patients with mild to moderate symptoms. Adult patients were randomly assigned to groups that consumed SCD or MD diet. The primary outcome of the study was symptomatic remission at week 6. Other end points included fecal calprotectin response and C-reactive protein response.
At the end of the study, the percentage of participants who achieved remission was not higher in the SCD group. FC response was achieved in 34.8% of patients with SCD compared to 30.8% in patients with MD. CRP response was only achieved in 2 patients with SCD compared to 1 patient with MD. It was concluded that SCD does not produce significantly better clinical outcomes compared to MD. This, combined with the fact that SCD is harder to commit for patients, makes a compelling case for MD.
2022: Guselkumab for Treating Crohn’s Disease - This clinical trial aimed to evaluate the efficacy and safety of guselkumab, a selective p19 interleukin 23 antagonist for treating psoriatic arthritis and plaque psoriasis in patients with moderate to severe Crohn’s disease. 309 patients were randomized to four groups to receive intravenous guselkumab of varying doses; intravenous ustekinumab, or placebo. Clinical outcomes were measured using Crohn’s Disease Activity Index Score, clinical remission, clinical response, clinical biomarker response, and endoscopy response, among others.
Another endpoint was the safety profile of guselkumab vs placebo. A higher percentage of patients who received guselkumab improved their clinical response. Safety event rates were similar across both treatment groups. The researchers concluded that the guselkumab of varying dosages induced superior clinical and endoscopic outcomes with a good safety profile.
Who Are Some Of The Key Researchers and Institutions Conducting Crohn's Disease Clinical Trial Research?
Balfour Sartor, MD is a leading researcher who has contributed to improvements in the understanding of Crohn’s disease, its diagnosis, and treatment. In celebration of his decades of research, the National Liberty Museum recognized Sartor as a Healthcare Hero in the Field of Crohn’s Disease. In addition to Crohn’s disease, Sartor has also led research studies that improved treatment for various inflammatory bowel disease. Sartor is known for establishing gnotobiotic murine models to determine their mechanisms of action.
Crohn’s & Colitis Foundation is the foremost authority in research for curing Crohn’s disease. The foundation is engaged in clinical trials that aim to develop novel treatment modalities and diagnostic tools to improve the quality of life for patients. They have a multidisciplinary team of health practitioners and researchers who work together to conduct clinical research. The foundation’s collaborative approach to research allows them to expedite research and unravel more information about Crohn’s disease.
Jill Roberts Institute for Inflammatory Bowel Disease is a research center dedicated to understanding the pathophysiology of Crohn’s disease. The institute collaborates with the Jill Roberts Center to develop effective diagnostic tools and treatment plans for patients. Scientists at the research center are more interested in the relationship between gut microbes and inflammation, along with other factors such as genetic predisposition and immune system dysfunction. Their researchers have engaged in a number of clinical trials to develop robust treatment programs for Crohn’s disease.
The Meyerhoff Inflammatory Bowel Disease Center has a multidisciplinary team of researchers dedicated to improving quality of life outcomes in patients with Crohn’s disease and other inflammatory bowel diseases. Their team of specialists includes leading researchers in gastroenterology, nurse practitioners, surgeons, and dieticians. The center has conducted a wide range of studies to discover new drug therapies and also understand the genetic and environmental causes of Crohn’s disease.