Pancreatic Cancer Survival Rate
What is Pancreatic Cancer?
Pancreatic cancer is characterized by the mutation and abnormal growth of cells in the pancreas, a small leaf-like gland sitting under the liver between the stomach and the spine.
For those who may not know, the pancreas produces enzymes that help with digestion as well as hormones for blood sugar management. It is the gland that produces the infamous insulin.
Pancreatic cancer may be rare by definition, but it is the 4th leading cause of cancer deaths. What makes it more troubling is that both its prevalence and death rate has been slowly increasing for the past several years.
According to the Pancreatic Cancer Action Network, a pancreatic cancer-focused non-profit organization commonly referred to as PanCAN, over 64,000 new cases of pancreatic cancer will be diagnosed in the US during the year 2023. That’s at least 175 new cases every day.
Types of Pancreatic Cancer
There are several types of pancreatic cancer, but they can broadly be grouped into two main categories based on the type of cell they originate in.
1. Exocrine Tumors
The majority – 93%to 95% - of pancreatic tumors are exocrine in nature. This means they start in the exocrine cells that make digestive enzymes. Pancreatic exocrine tumors are further subdivided into the following types:
Adenocarcinoma –More than 90% of all pancreatic cancers are adenocarcinomas, making it the most common type. Pancreatic adenocarcinomas start in the cells in the pancreatic duct lining.
Other types of pancreatic exocrine tumors include:
- Acinar Cell Carcinoma
- Squamous Cell Carcinoma
- Adenosquamous Carcinoma
- Colloid Carcinoma
Apart from adenocarcinoma, all types of exocrine tumors of the pancreas are rare.
2. Neuroendocrine (endocrine) Tumors
Formally called Pancreatic Neuroendocrine Tumors or PNETs in short, these types of tumors are found in about 7% of pancreatic cancer cases. As the name suggests, these types of tumors develop in the endocrine cells of the pancreas, which are called islet cells. Hence, they are sometimes referred to as islet cell tumors as well.
Endocrine or islet cells are responsible for making hormones that regulate blood sugar.
Most PNETs are non-functional, i.e., they do not produce hormones, but some are functional, meaning they continue to produce hormones just like normal cells.
PNETs are classified into different types based on the hormones the affected cells make. These include:
- Insulinoma –Insulin cells
- Gastrinoma – Gastrin cells
- Glucagonoma – Glucagon-making cells
- VIPoma – Cells that make vasoactive intestinal peptide.
- Somatostatinoma – Somatostatin-producing cells.
- Non-Functional Islet Cell Tumor – Grows in endocrine cells of the pancreas that do not make any hormone.
What are the Signs and Symptoms of Pancreatic Cancer?
Most often than not, pancreatic cancer doesn’t cause any symptoms until it has progressed to an advanced stage. Even then, the majority of pancreatic cancer symptoms are non-specific. These may include:
- Jaundice
- Abdominal/stomach/back pain
- Changes in stool
- Unexplained weight loss
- Indigestion
- Feeling sick
- Diabetes (when the disease affects insulin-producing cells)
- Itchy skin
- Dark urine
- Fatigue
- Nausea and vomiting
Pancreatic Cancer Diagnosis and Staging
Unlike breast cancer, there is no screening test for pancreatic cancer. This means you cannot be routinely screened for it. Doctors typically only examine/scan/test patients for pancreatic cancer when they exhibit some symptoms, which (as discussed in the previous section) does not usually happen until the disease has progressed significantly.
For these two main reasons, pancreatic cancer is usually diagnosed at later stages.
How is Pancreatic Cancer Diagnosed?
The absence of screening and diagnostic procedures requires doctors to perform a few things to determine if someone has pancreatic cancer. This includes:
- Imaging Tests (one or more) – Transabdominal or Endoscopic Ultrasound, CT scan, MRI, PET Scan, ERCP, or Laparoscopy.
- Blood Work – May include testing for pancreatic tumor markers, like CA 19-9, CEA, cgA, and PP.
- Urine and stool tests
- Physical exam
- Tissue sampling (Biopsy)
Pancreatic Cancer Staging
The diagnosis of pancreatic cancer is followed by a series of more tests to determine the type, grade, and stage of cancer. This is essential to laying out the best treatment plan.
The tissue samples of the tumor taken in biopsy help determine the type and grade of cancer, whereas imaging tests, like PET scan, CT scan, and MRI, show how far the disease has spread in the body.
Like other cancers, the staging of pancreatic cancer is done using the TNM Staging System.
TNM Staging of Pancreatic Cancer
TNM stands for:
- T –Tumor – corresponds to the size and depth of the tumor
- N – Node – states whether cancer has spread to the lymph nodes. If yes, how much.
- M – Metastasis – describes if cancer has spread to distant parts of the body.
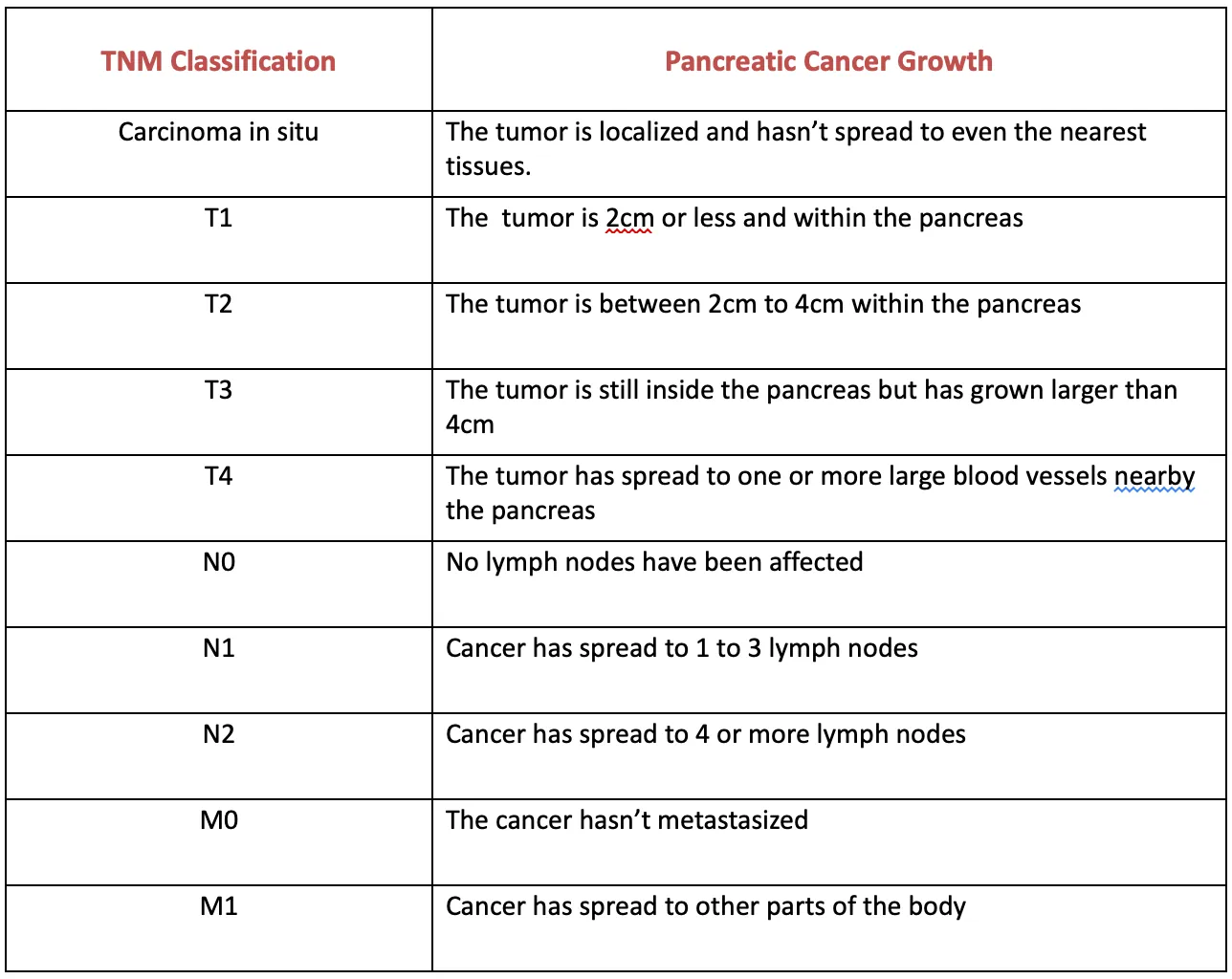
Numerical Stages of Pancreatic Cancer
The more easily understood by patients (and the general public), numerical stages are determined on the basis of TNM staging. These include:
- Stage 0 – Abnormal cells are detected in the pancreas lining.
- Stage I – Cancerous tumor is found, but it is confined in the pancreas
- Stage II – Cancer has started to spread to nearby areas. Late stage II is characterized by the spread of cancer to nearby lymph nodes.
- Stage III – The cancer cells have spread to surrounding tissues, organs, major blood vessels, and lymph nodes.
- Stage IV – Cancer has metastasized, i.e., spread to distant tissues and organs. It may have also spread to distant lymph nodes.
Is Pancreatic Cancer Hereditary?
Certain gene mutations that can be inherited put you at an increased risk of pancreatic cancer. These are the same gene mutations associated with breast cancer – BRCA1 and BRCA22.
According to research, about 10% of pancreatic cancer cases are due to these inherited BRCA gene mutations.
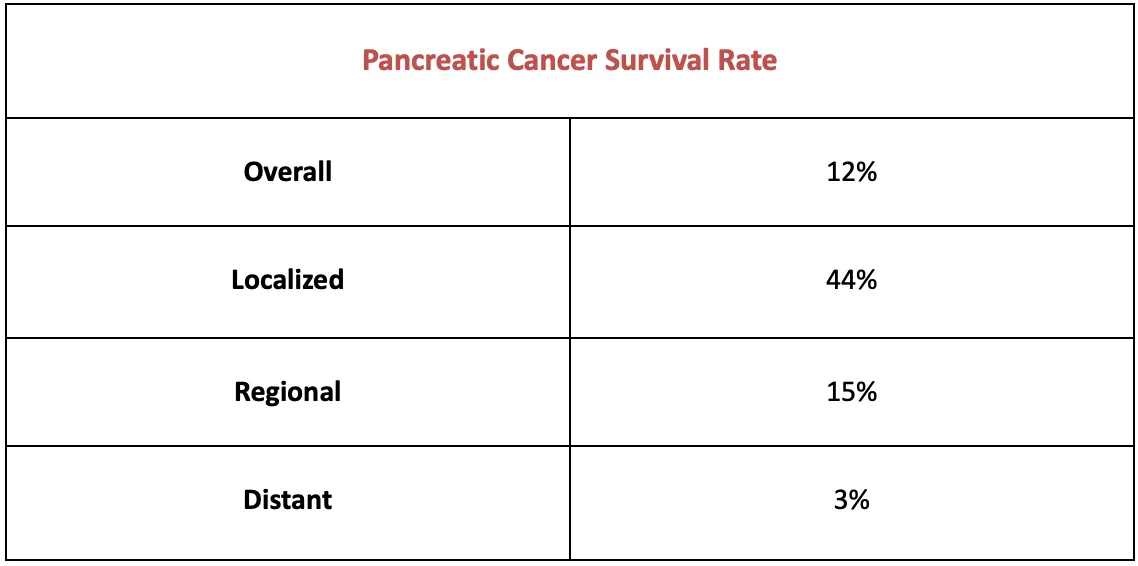
Pancreatic Cancer Survival Rate
Since pancreatic cancer is usually detected at an advanced stage, it has a poor prognosis. However, it has gradually improved over the years.
As reported in American Cancer Society’s Cancer Facts & Figures 2023, the 5-year survival rate for pancreatic cancer has increased from 3% in 1975-77 to 12% in 2012-2018. The improvement has been slow, but it shows that there’s hope. And considering the rapid advancements in medical science happening now, we can expect further improvements in the upcoming years.
Pancreatic cancer may not have a good overall prognosis. But it’s important to remember that survival rate statistics only provide an average percentage. While they do provide an outlook for how the disease affects most people, it doesn’t guarantee that every pancreatic cancer patient will have the same journey. One may live much longer than many other patients if diagnosed earlier, responds well to treatment, has a healthy lifestyle, and is in good overall health.
It’s also important to note that these survival statistics are measured every five years. This means that they may not always paint an accurate picture of the improvements made during the past few years in pancreatic (or any) cancer diagnosis and treatment.
What is the Survival Rate for Pancreatic Cancer?
The overall 5-year survival rate of pancreatic cancer is 12% in the US.
However, if detected at an early stage, which happens in only about 15% of cases, the survival rate increases to 44%.
Among those diagnosed with pancreatic cancer when it has already spread to surrounding organs, the 5-year survival rate is known to be 14%. And those who learn about their disease when cancer has already metastasized, i.e., spread to distant organs, have a 5-year survival rate of 3%.
Average Survival Rate for Pancreatic Cancer
According to John Hopkins Medicine, patients diagnosed with pancreatic cancer at stage IV live for about 1 year on average. For patients diagnosed at an early or middle stage – when cancer hasn’t spread much in the body – the average survival rate is 3 to 3.5 years.
Survival Rate for Resectable Tumors
Resectable tumors can be surgically removed. This is usually only possible with localized pancreatic tumors (stage I and II). However, it might be (rarely) an option for some stage III locally advanced pancreatic tumors.
Surgery is seldom a cure for pancreatic cancer, and the tumor can grow back in some time.
Around 15% to 20% of pancreatic tumors are resectable, and the 5-year survival rate for these patients (after surgery) is 20% to 30%. On average, patients with resected pancreatic tumors live for about 2.5 years.
Pancreatic Cancer Treatment Options
Surgery, chemotherapy, and radiation therapy are the three key treatments available for pancreatic cancer.
However, surgery is not an option for most patients. As discussed earlier, pancreatic cancer is mostly diagnosed at a later stage (when it has already started to spread), making surgery impossible. For these patients, doctors may combine chemotherapy with targeted drug therapy to slow the progression of the disease and help patients live longer.
Immunotherapy is another treatment option for cancers, but only a small number of pancreatic cancer patients qualify for it.
How is Pancreatic Cancer Treated?
For most pancreatic cancer patients, treatment involves chemotherapy because it has already grown to an advanced stage. However, surgery may be the first step to treating the disease for the small number of patients whose cancer is diagnosed at an early stage.
Here’s a quick overview of what pancreatic cancer treatment may look like for patients at different stages:
Early Stages (I and II)
- Surgery
- Chemotherapy
- Radiation (sometimes)
Late Stages (III and IV)
- Chemotherapy
- Targeted Drug Therapy
- Immunotherapy
Precision Medicine
Precision Medicine is an emerging field in pancreatic cancer treatment. It involves determining the best treatment approach/drugs based on each patient’s biology through genetic and biomarker testing for inherited mutations and the tumor’s unique genetic makeup and biological characteristics.
According to the latest research, treating pancreatic cancer through precision medicine helps patients live one year longer on average than those treated through standard procedures.
Clinical Trials for Pancreatic Cancer
Clinical trials are never the first line of treatment for pancreatic cancer (or any disease, for that matter). They are only recommended when the disease displays a unique growth pattern, or the patient doesn’t respond well to standard treatments.
There are multiple online platforms that patients and their families can use to find clinical trials for pancreatic cancer. Some of the most reliable ones include:
Risk Factors for Pancreatic Cancer
A number of health and lifestyle factors can increase your risk for pancreatic cancer. While some are beyond one’s control, others can be managed by lifestyle improvements. These include:
- Inherited gene mutations (BRCA1 and BRCA2)
- Certain genetic syndromes, like Lynch syndrome.
- Smoking – Smoking makes you twice as likely to develop pancreatic cancer as non-smokers
- Excess body weight
- Excessive alcohol consumption
- Diabetes (type 2)
Conclusion
Pancreatic cancer (unfortunately) has a poor prognosis. This is due to the disease being usually diagnosed at a later stage. While there’s no screening test for pancreatic cancer, regular medical exams may help doctors detect any changes in your health or reports, leading them to further testing, which then may help find the disease at an early stage.
Pancreatic cancer is seldom curable, but its early diagnosis helps improve the prognosis. Early detection is also associated with a longer survival probability. So, don’t miss your medical appointments.